
Skin Cancer Screenings and Treatment
According to the American Academy of Dermatology, skin cancer is the most common form of cancer in the United States. Given the fact that 1 in 5 people will be diagnosed with skin cancer during their lifetime, and there are many different types of skin cancer, it’s imperative that everyone is screened regularly for this disease which can be deadly. Early detection often leads to a higher success rate with treatment.
Basal Cell Carcinoma
Basal cell carcinomas (BCC) are the most common and mildest form of skin cancer. There are some invasive or more aggressive types of basal cells too, but usually basal cell carcinomas just sit on the surface of the skin and grow there. They do not tend to spread to other organs like lymph nodes or the brain. In general, they are usually easy to treat and cure, especially if they are found early.
Signs and symptoms to be aware of:
- Waxy pink and pearly bump
- May have central scab or erosion
- Often look like a pimple or a bug bite
- Difficulty healing
- May look like a patch of eczema or psoriasis that does not respond to steroid creams
- On sun-exposed areas of the skin
Risk factors:
- Ultraviolet light exposure from the sun or tanning bed use
- Fair skin
- Over the age of 50 years
- History of previous BCC or other types of skin cancer
- Chronic skin inflammation from previous injuries like burns or scars
Treatment options:
- Electrodesiccation and curettage: A small curette is used to scrape out the skin cancer and a hyfrecator is used to denature the remaining cells. Also known as the scrape and burn method
- Surgical excision: Cut out the skin cancer and close with stitches performed by our Dermatology providers or Plastic Surgeon
- Prescription Creams: used at home to treat superficial skin cancer, when surgery is not appropriate
- Mohs Surgery: A special type of skin cancer surgery reserved for skin cancers on certain areas of the body, like the head and neck. Specially trained dermatologic surgeons perform Mohs


Squamous Cell Carcinoma
Squamous cell carcinomas (SCC) are the second most common form of skin cancer.
They can be superficial (SCC in-situ) or invasive. Unlike basal cell carcinomas, more invasive SCCs can metastasize or spread to other organs.
Signs and symptoms to be aware of:
- Thick, flesh-colored to red crusty bump or patch
- Typically arises on sun-exposed skin but can occur on lips, genitals, and non-exposed skin
- Often look like a wart or a skin tag
- Can be superficial or invasive
Risk factors:
- Ultraviolet light exposure from the sun or tanning bed use
- Fair skin
- Over the age of 50 years
- History of previous SCC or other types of skin cancer
- Chronic skin inflammation from previous injuries like burns or scars
- Immunosupressive medications, like from organ transplant surgery or certain illnesses
- History of the human papilloma virus (HPV)
Treatment options:
- Surgical excision: Cut out the skin cancer and close with stitches performed by our Dermatology providers or Plastic Surgeon
- Electrodesiccation and curettage: A small curette is used to scrape out the skin cancer and a hyfrecator is used to denature the remaining cells. Also known as the scrape and burn method
- Prescription Creams: used at home to treat superficial SCC-in situ, when surgery is not appropriate
- Mohs Surgery: A special type of skin cancer surgery reserved for skin cancers on certain areas of the body, like the head and neck. Specially trained dermatologic surgeons perform Mohs
- In the case of more severe or invasive skin cancers, we may need to refer out for more extensive treatments including chemotherapy or radiation
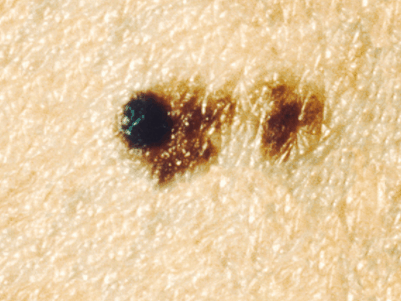
Melanoma
Melanoma is the most serious type of skin cancer.
Most of the time melanomas are very dark in color, but occasionally they are pink and look more like BCCs.
Signs and symptoms to be aware of:
- Asymmetrical; one half of the mole does not match the other
- Border irregularity
- Color is not uniform including colors like black, brown, gray, blue and white
- Diameter greater than a pencil eraser (6 mm) is more suspicious
- Evolving shape, color or size; spots that change are more suspicious
Risk factors:
- Biggest risk factor = Ultraviolet radiation from either the sun or tanning bed use
- Fair skin
- Compromised immune system
- History of other skin cancers or a previous melanoma
- Having many moles; the more moles you have and the bigger your moles are, the greater the chance of developing a melanoma
- Family history and genetics also play a role in your risk for melanoma
Treatment options:
We prefer to catch them when they are smaller, but the depth of the lesion is more important than the diameter. A special type of biopsy is performed when we suspect melanoma to get under the entire spot instead of just testing a small piece. We usually do what is called an “excisional biopsy” which will require stitches. If the results come back positive for melanoma, depending on how deep the mole was according to the dermatopathologist who analyzes it under the microscope, you will either simply need another larger excision or you will need to have lymph nodes removed to see if the cancer has started to spread to other areas. Sometimes additional blood testing or scans such as MRIs, CTs and PET scans are needed.
Very important to monitor:
Skin cancers can recur even after they have been removed properly. After one skin cancer, the risk of having another significantly increases. It is important to follow up with your dermatology provider every 6 to 12 months to make sure the site is still healed and also to check for new spots. It is also important to take proper sun avoidance precautions to protect yourself from further sun damage that could cause more skin cancers.
What is an Atypical Mole?
Dermatologists will often biopsy a mole because it looks “atypical.” It often has at least one or two of the ABCDEs of Melanoma. There is a spectrum of atypical moles:
Does not need further treatment as these do not seem to have much of an increased risk for turning into melanoma. It is important to keep an eye on the rest of your moles and if new ones pop up or old moles change, we will probably be more likely to biopsy them.
Usually recommended to remove entirely. Also do not have a huge risk of turning into cancer but if the mole grows back partially it will appear misleadingly more suspicious down the road.
Must be completely removed as these do have a higher chance of turning into melanoma. May be treated like a melanoma.
Large excision is warranted to guarantee the entire cancer is removed including any adjacent invasion. Lymph nodes may also need to be removed and tested depending on the depth.
When in doubt, get it checked out! If you have any spots that sound like the above descriptions, or any spots that have changed and look different from how they looked a few months or years ago, then schedule an appointment for a total body skin examination to get those spots and all of your other spots evaluated to see if they need a biopsy.
